How We’re Mitigating Life
Threatening Complications
Due to Acute Pancreatitis

How We’re Mitigating
Life-threatening
Complications Due to
Chronic Pancreatitis
Acute Pancreatitis represents an unmet need in critical care medicine as there are no approved disease-modifying therapies.
Reduction in new onset respiratory failure
Reduction in severe organ failure
Reduction in necrotizing pancreatitis
Reduction in hospital stays > 21 days
Acute Pancreatitis
with SIRS
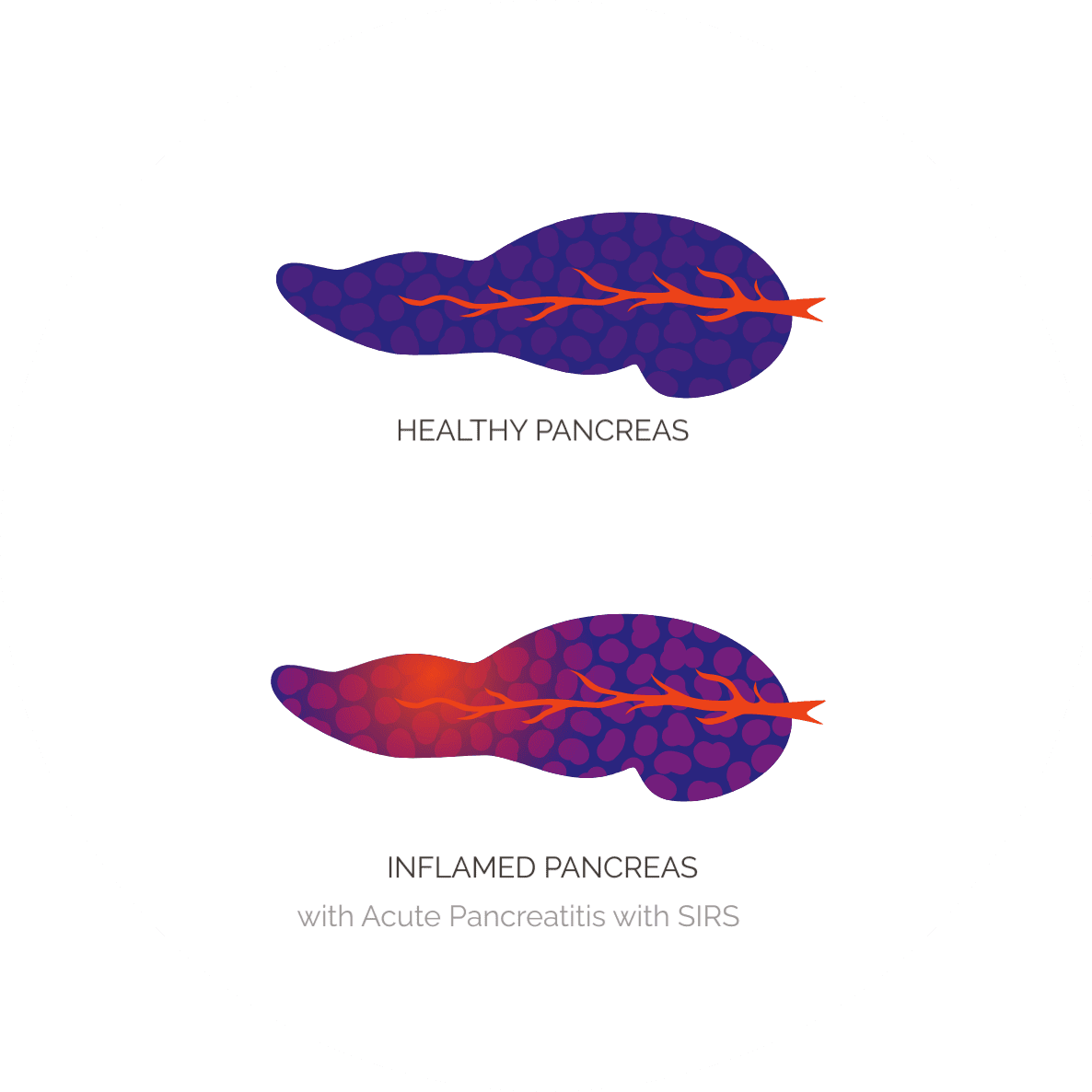
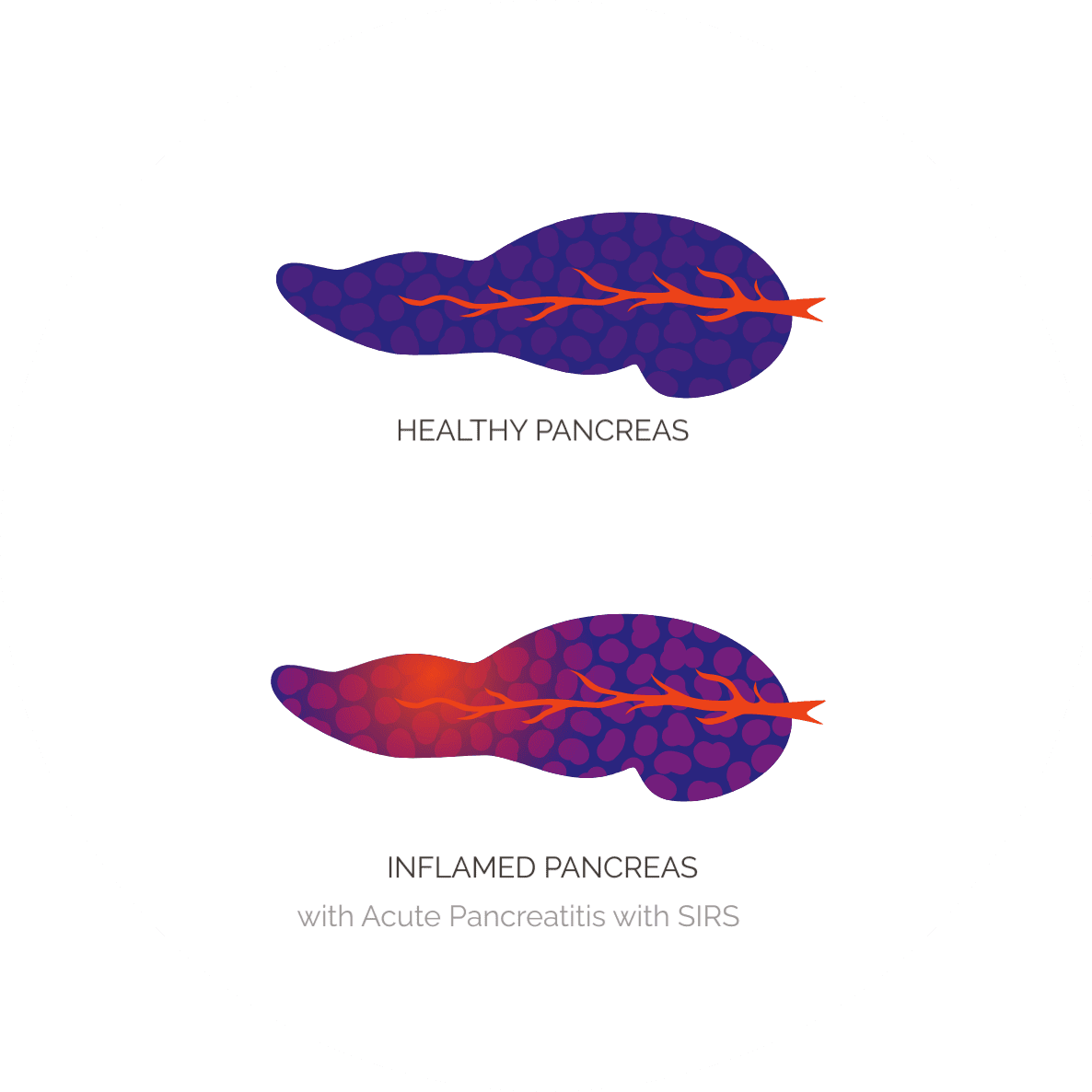
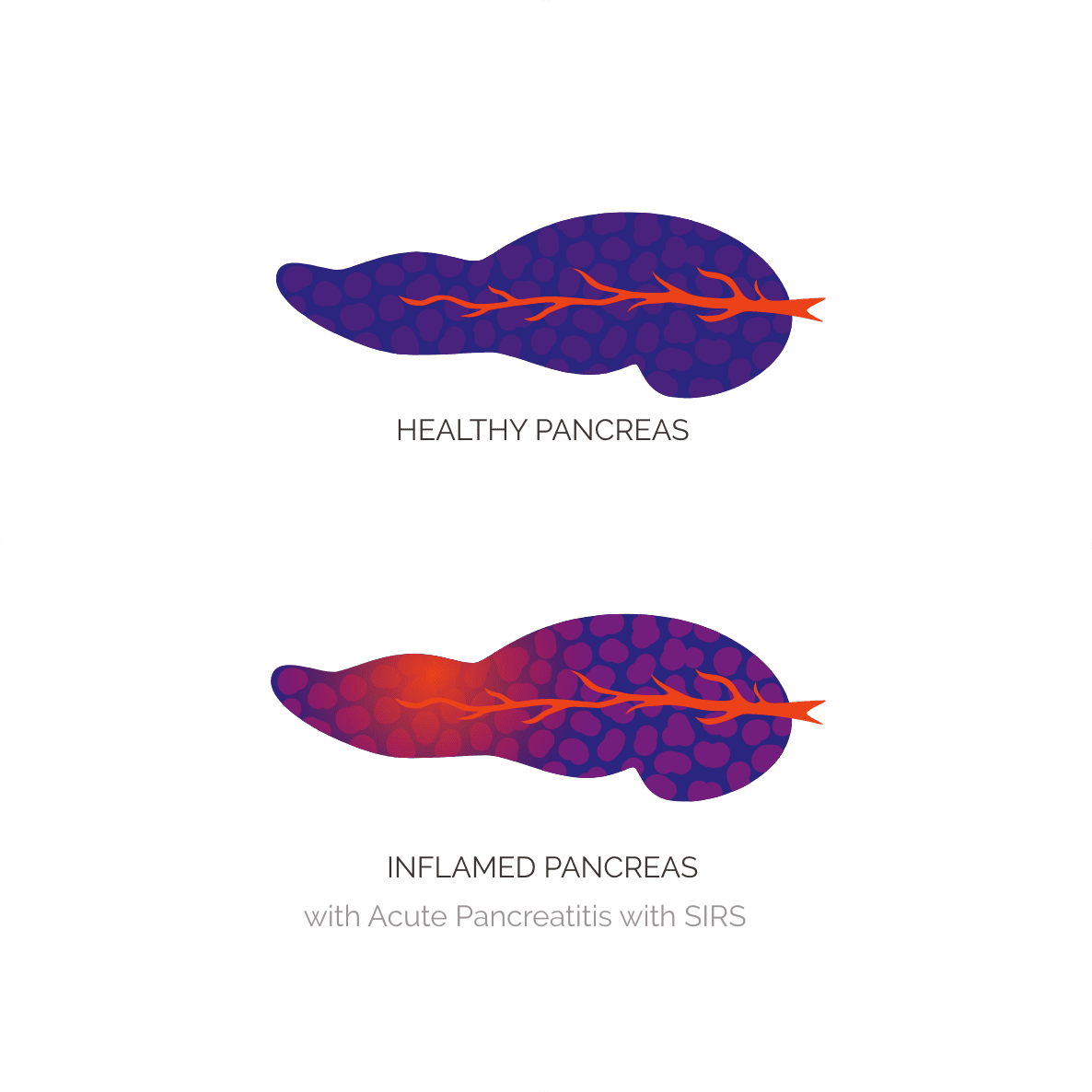
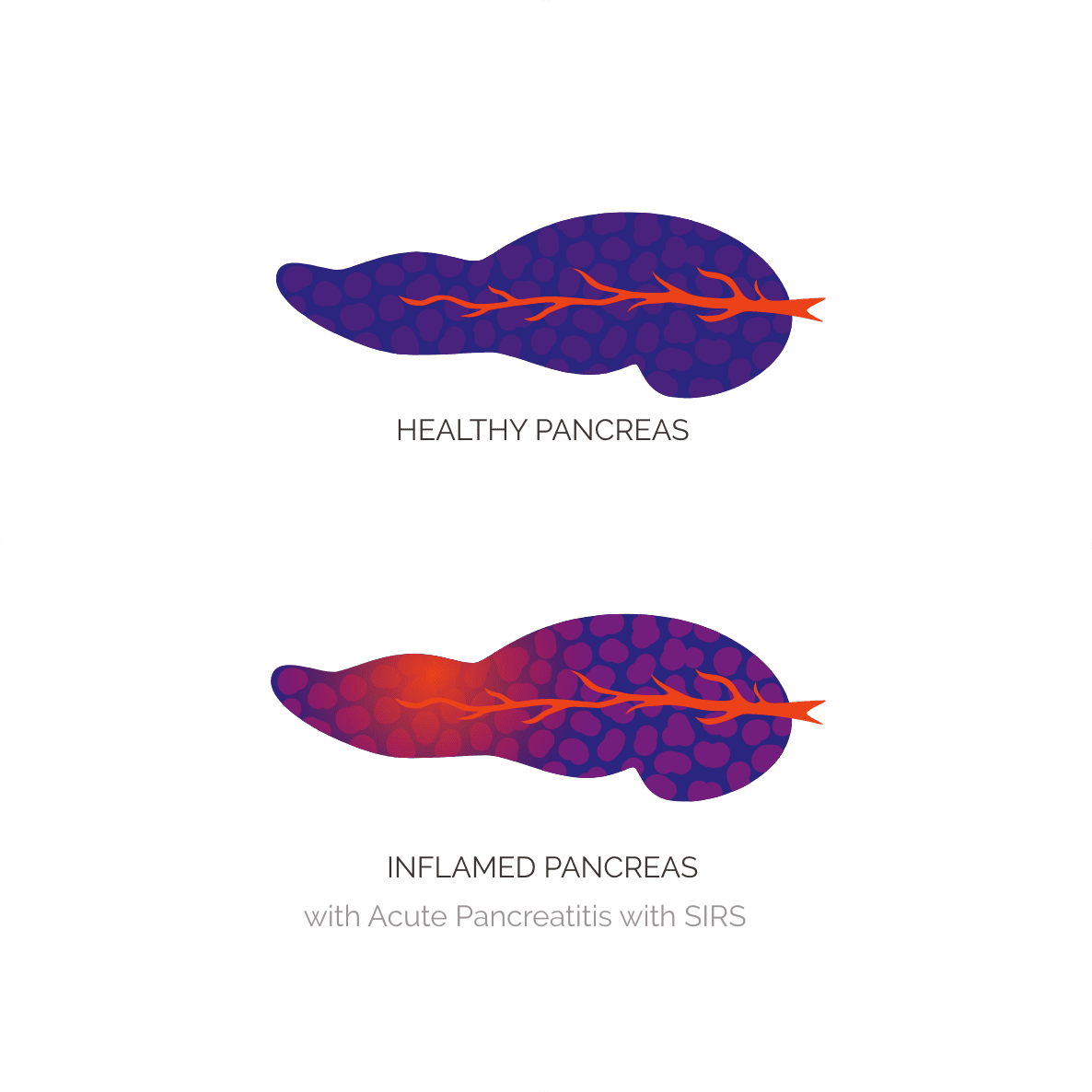
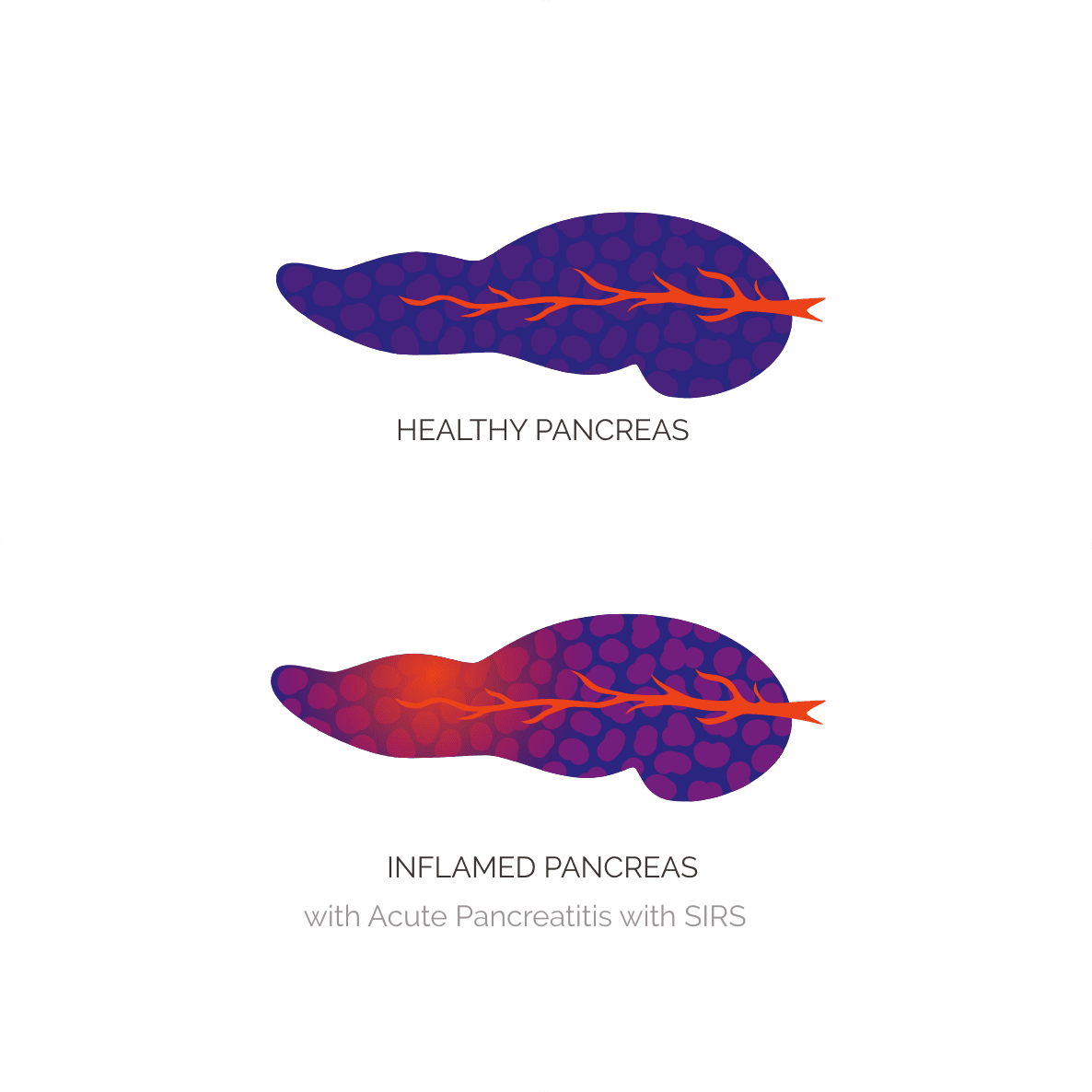
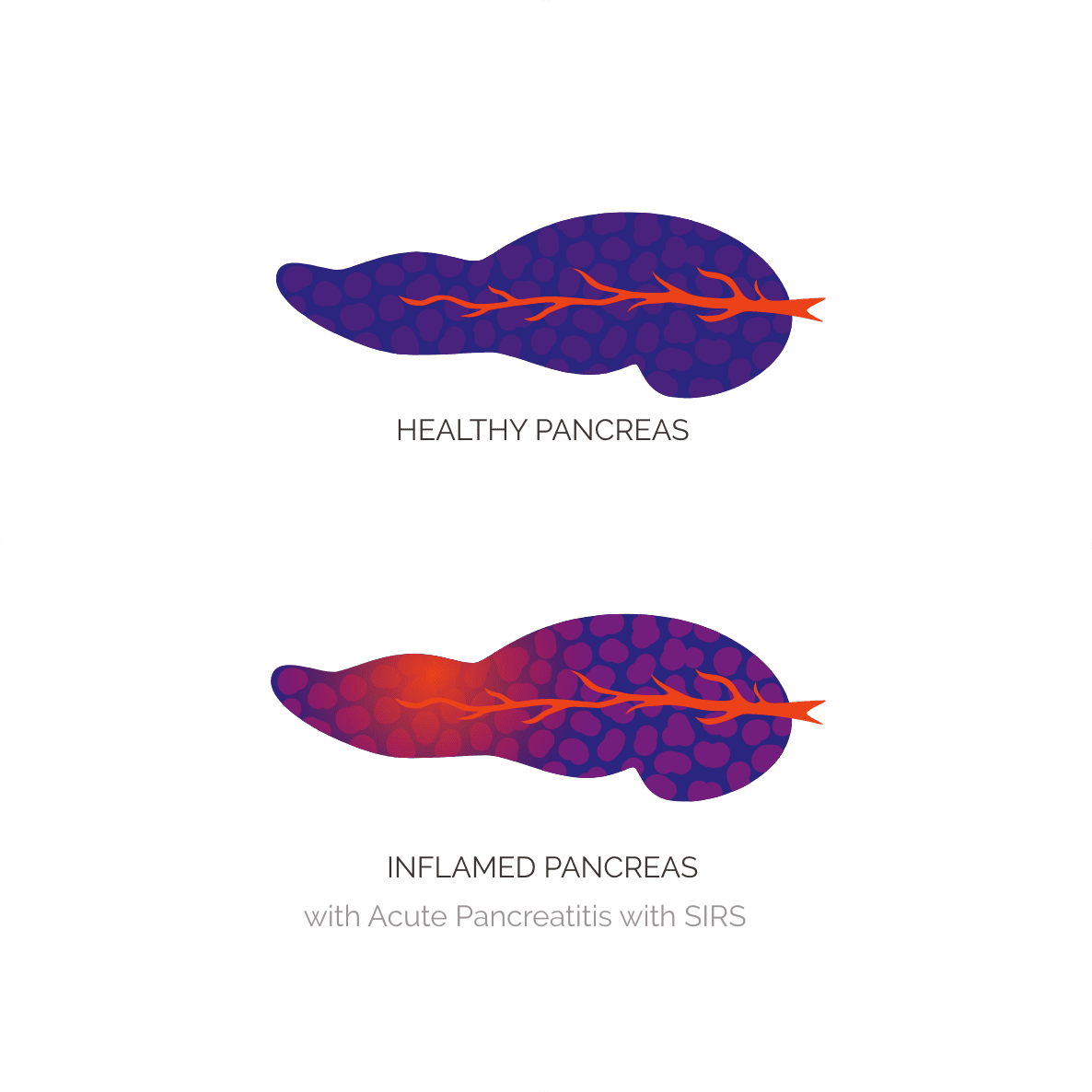
Acute pancreatitis (AP) is an acute inflammatory process of the pancreas that presents as severe upper abdominal pain, often accompanied by nausea and vomiting. During episodes of the disease, inflammation of the pancreas occurs, which can lead to pancreatic cell death or necrosis and systemic inflammation. Normal pancreatic functions, such as the secretion of digestive enzymes into the gut that are required to break down proteins, carbohydrates and fats, are compromised.
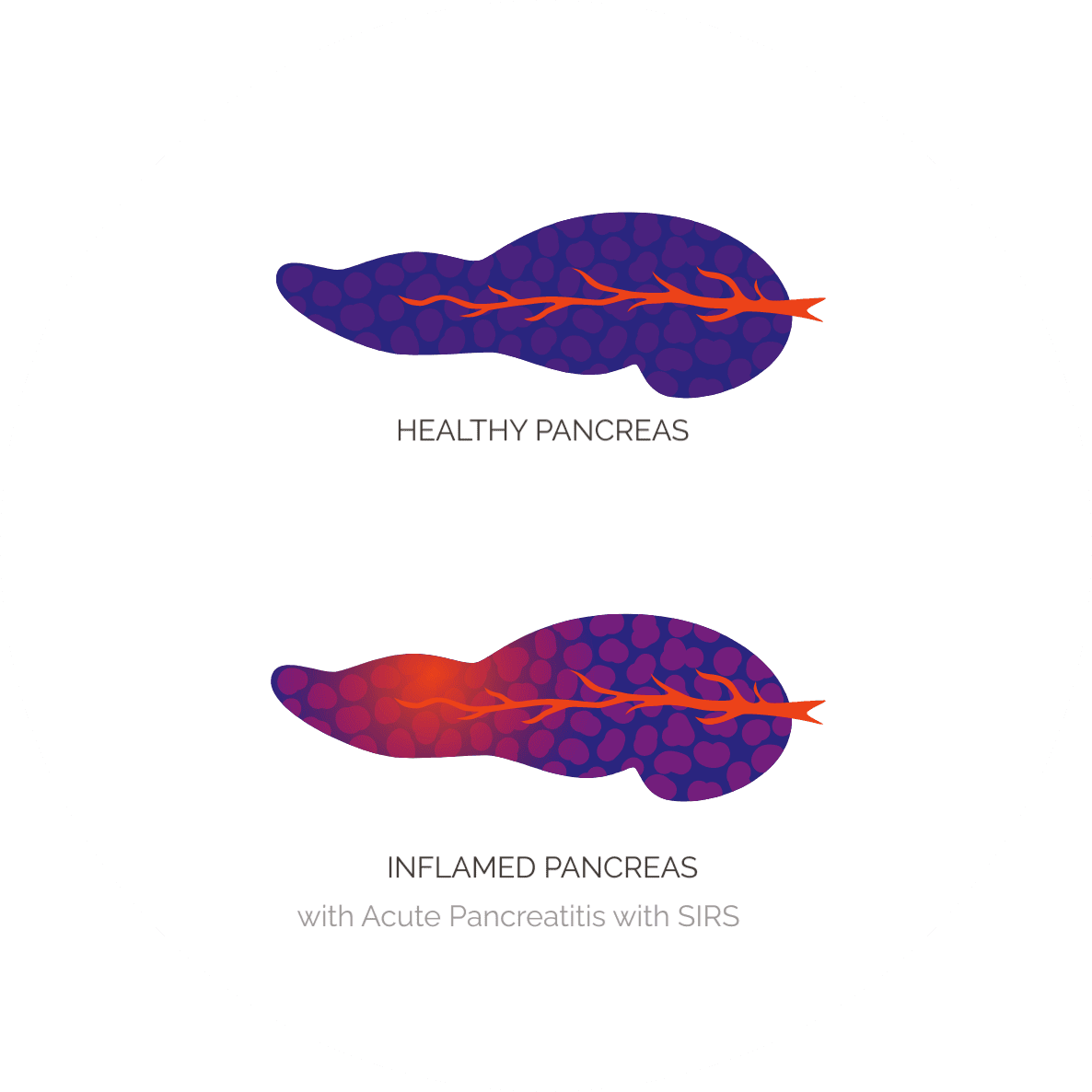
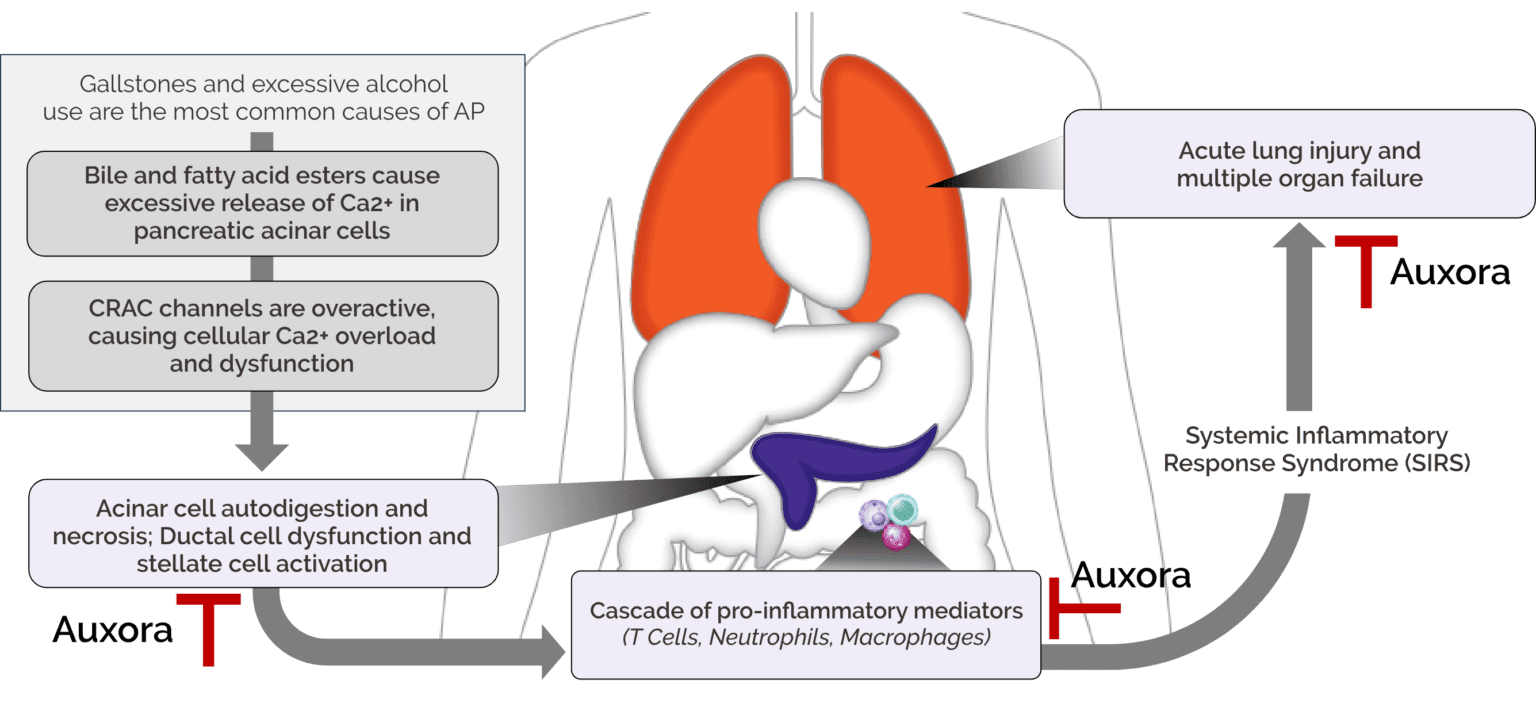
The challenge for AP is that severe complications can arise because of the acute inflammatory response that occurs in the pancreas. One serious complication is Systemic Inflammatory Response Syndrome, or SIRS, which can lead to failure in organs beyond the pancreas, including the lung. AP patients who have SIRS at diagnosis are more likely to develop life-threatening severe AP than patients without SIRS.
There are no approved therapeutics for AP.
Hospitalizations per year for AP
Over 100,000 hospitalizations per year for AP with SIRS
With severe AP
Auxora in Acute Pancreatitis
Our Clinical Studies in AP
Acute Pancreatitis Phase 2a Clinical Trial
Study Design
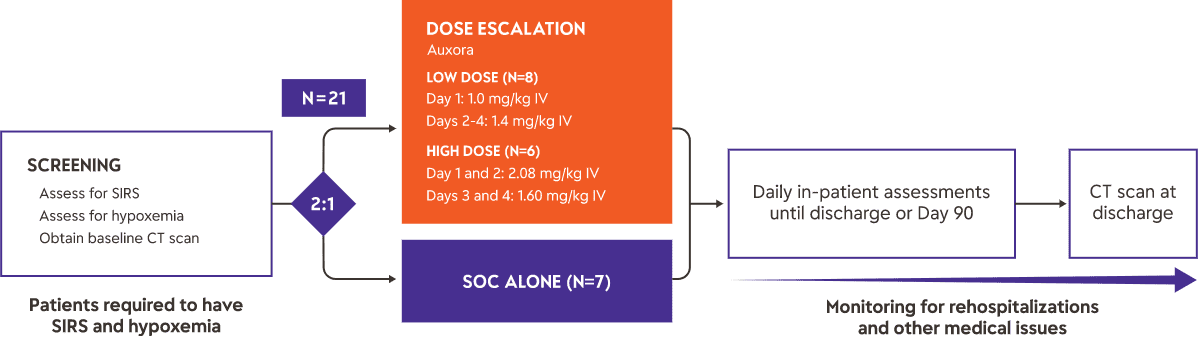
We completed a Phase 2a clinical trial of Auxora™ in 21 patients with AP with predicted severe disease as determined by the presence of SIRS and hypoxemia. Fourteen patients received Auxora™ plus standard of care, typically aggressive fluid resuscitation and pain medication, at two different dose levels, and seven received standard of care only. The Auxora™ treated patients received a daily IV dose of Auxora™ for up to four days. As an early-stage proof of concept trial, this trial was not powered for statistical significance for any of the endpoints.
Results
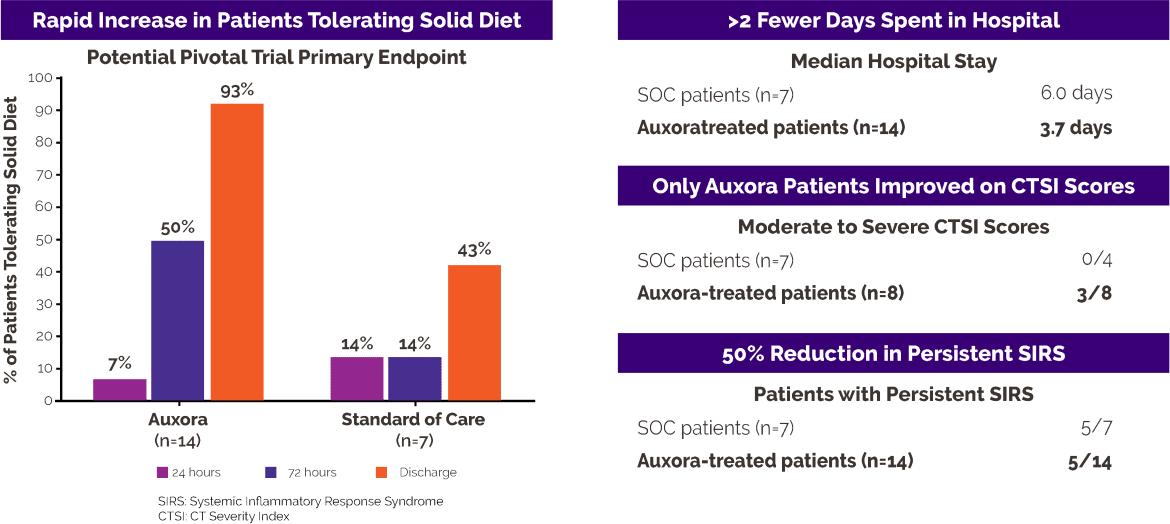
The primary symptom associated with AP is severe upper abdominal pain. Patients with AP are unable to tolerate any solid food without an increase in pain or the occurrence of nausea or vomiting until the pancreatitis resolves. In this clinical trial, only one patient in the Auxora™ treated group (7%) and one patient in the SOC group (14%) were tolerating solid food at study entry. After 72 hours, seven of 14 (50%) Auxora™ patients were tolerating solid food while only one of seven standard of care patients was tolerating solid food. At the time of hospital discharge, 13 of 14 (93%) Auxora™ patients could tolerate solid food compared to three of seven (43%) SOC patients.
Patients treated with Auxora™ were discharged from the hospital after a median of 3.7 days compared to SOC patients, who had a median stay of 6.0 days.
Persistent SIRS, defined as SIRS lasting more than 48 hours, is an indication of continued activation of inflammatory pathways in patients with AP, and SIRS is predictive for the development of organ failure. All patients in this AP trial had SIRS at enrollment. Only five of 14 patients (36%) treated with Auxora™ developed persistent SIRS, while five of the seven patients (71%) treated with SOC alone had persistent SIRS.
For more details on the clinical trial, please visit: A Study of Auxora in Patients With Acute Pancreatitis and Accompanying SIRS.
Information on our Expanded Access Policy can be obtained through the following link.
CARPO Phase 2b clinical trial in patients with AP and accompanying SIRS
Study Design
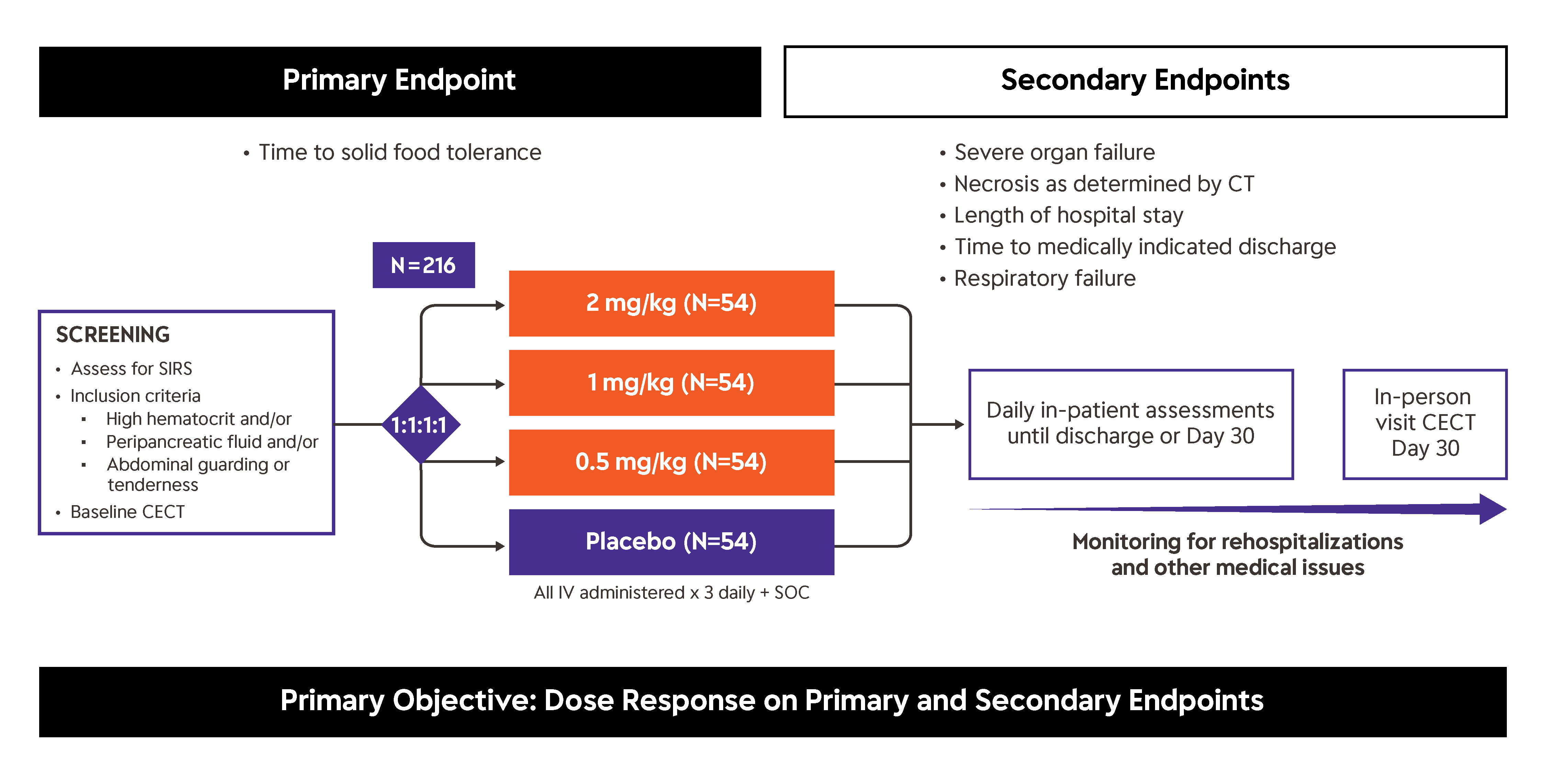
The target population for Auxora™ in the recently completed Phase 2b CARPO Clinical trial is AP patients with accompanying SIRS, which we estimate to be approximately 100,000 patients per year in the United States.
For more details on the clinical trial, please visit: A Study of Auxora in Patients with Acute Pancreatitis and Accompanying SIRS (CARPO).
Information on our Expanded Access Policy can be obtained through the following link.
Results
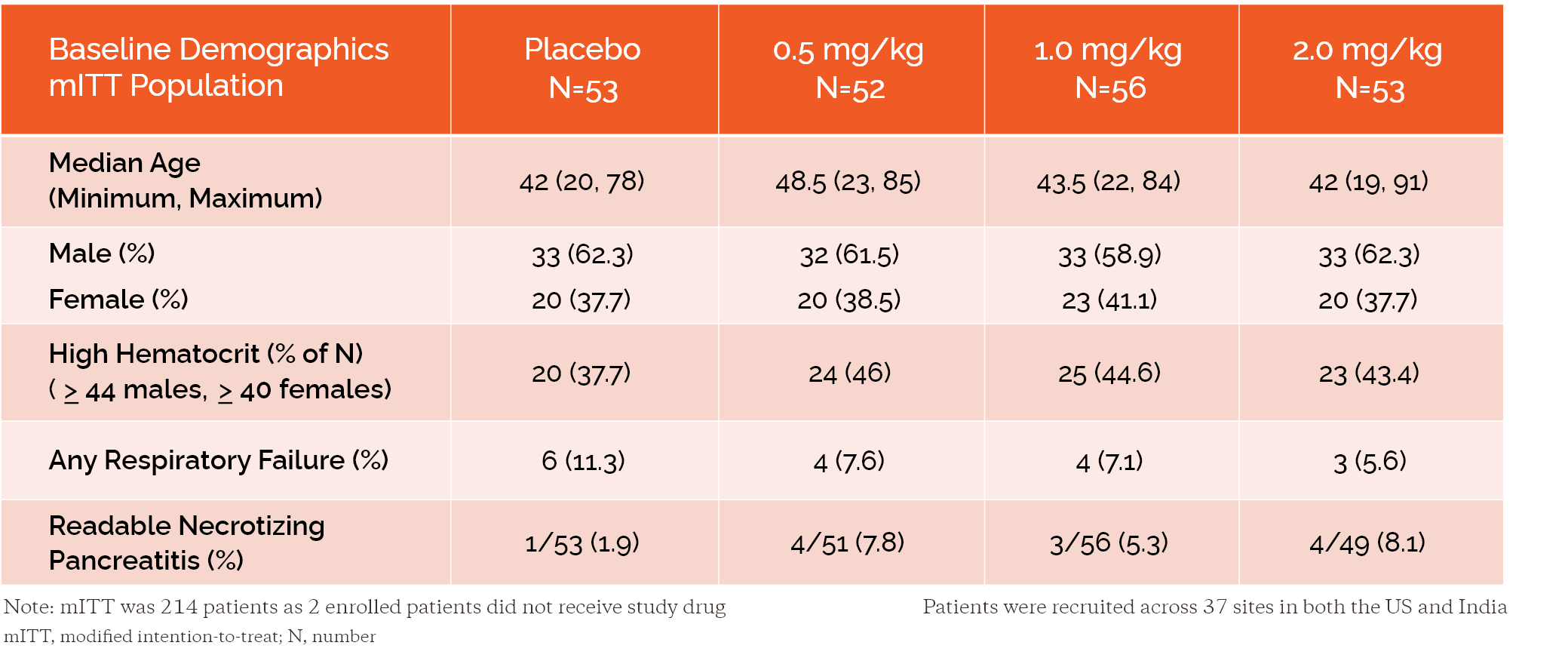
Baseline Characteristics were Generally Aligned Across Groups
Dose Response Observed for the Primary Endpoint
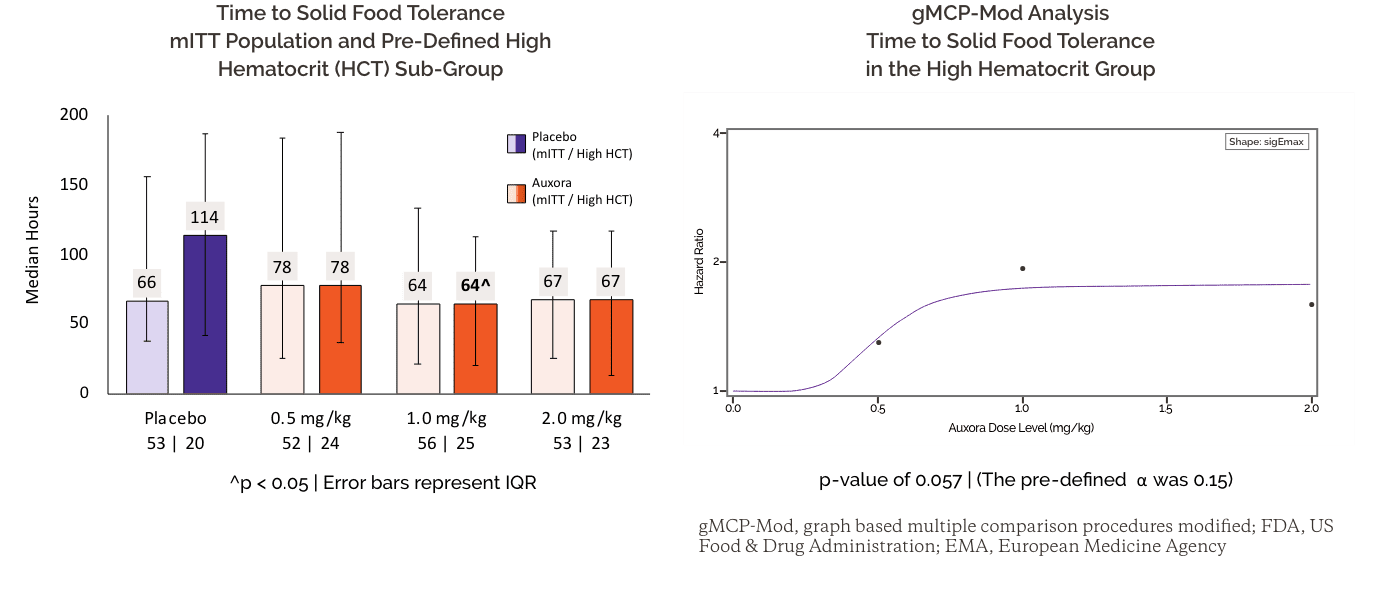
Auxora High and Medium-Doses Reduced All Types of Severe Organ Failure
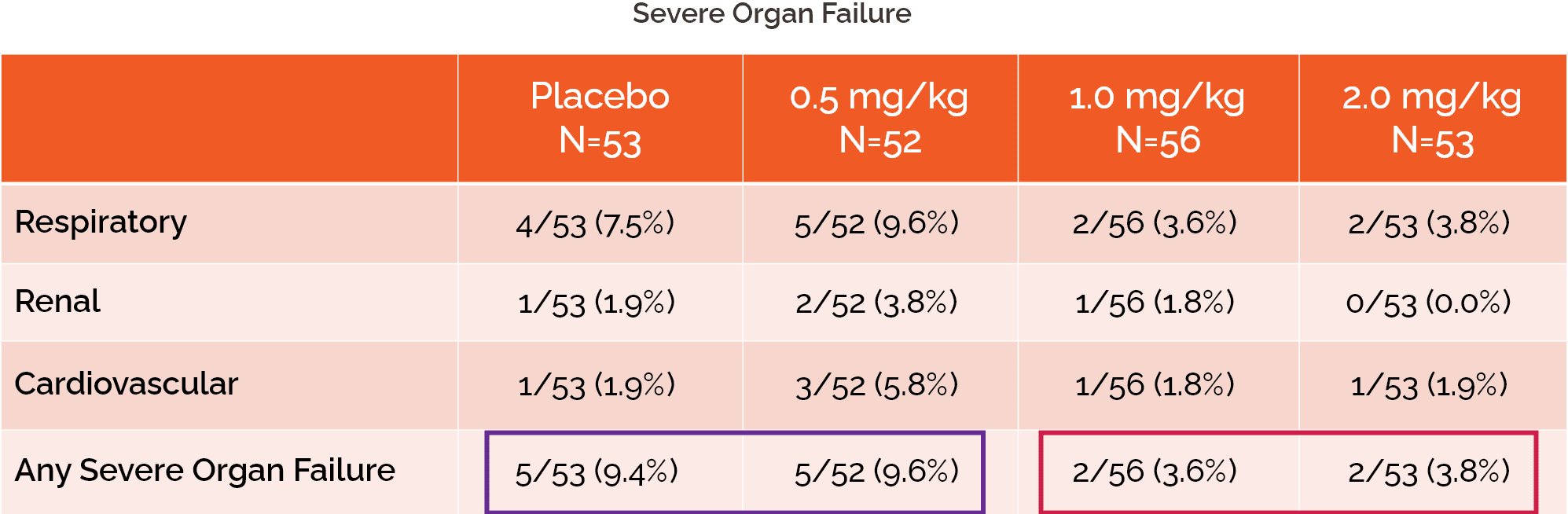
Severe Respiratory Failure: Receiving invasive mechanical ventilation (IMV) OR use of either high flow nasal cannula (HFNC) or non-invasive mechanical ventilation (NIMV) for ≥ 48 hours
Severe Renal Failure: Initiation of renal replacement therapy
Severe Cardiovascular Failure: Use of vasopressor or inotropic support for ≥48 hours
Dose Response Was Observed For Both New Onset Persistent and Severe Respiratory Failure
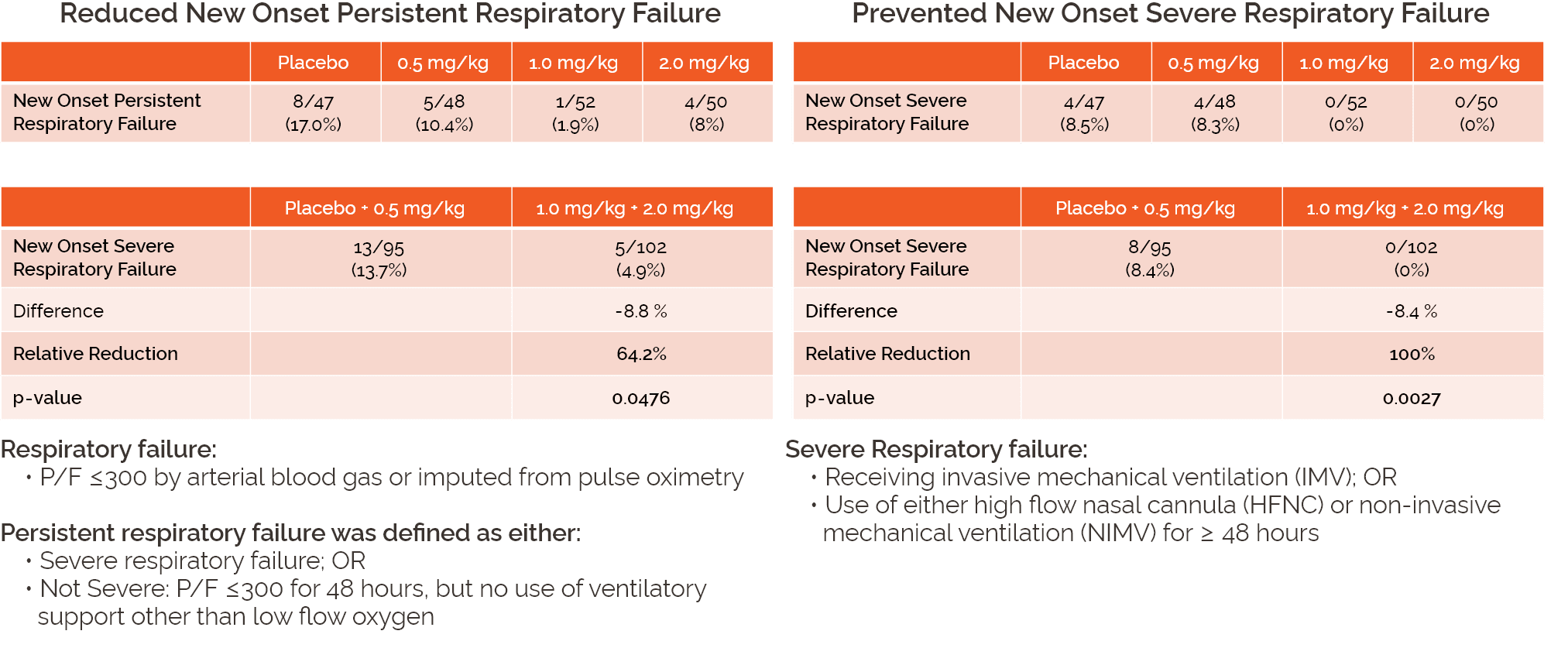
Differences were calculated using Cochran-Mantel-Haenszel test stratified by CRF recorded gender
(male or female) and the risk for hematocrit (HCT) (higher or lower) based on CRF data
Auxora High-Dose Demonstrated Improvements in Additional Key Secondary Endpoints within the mITT Population
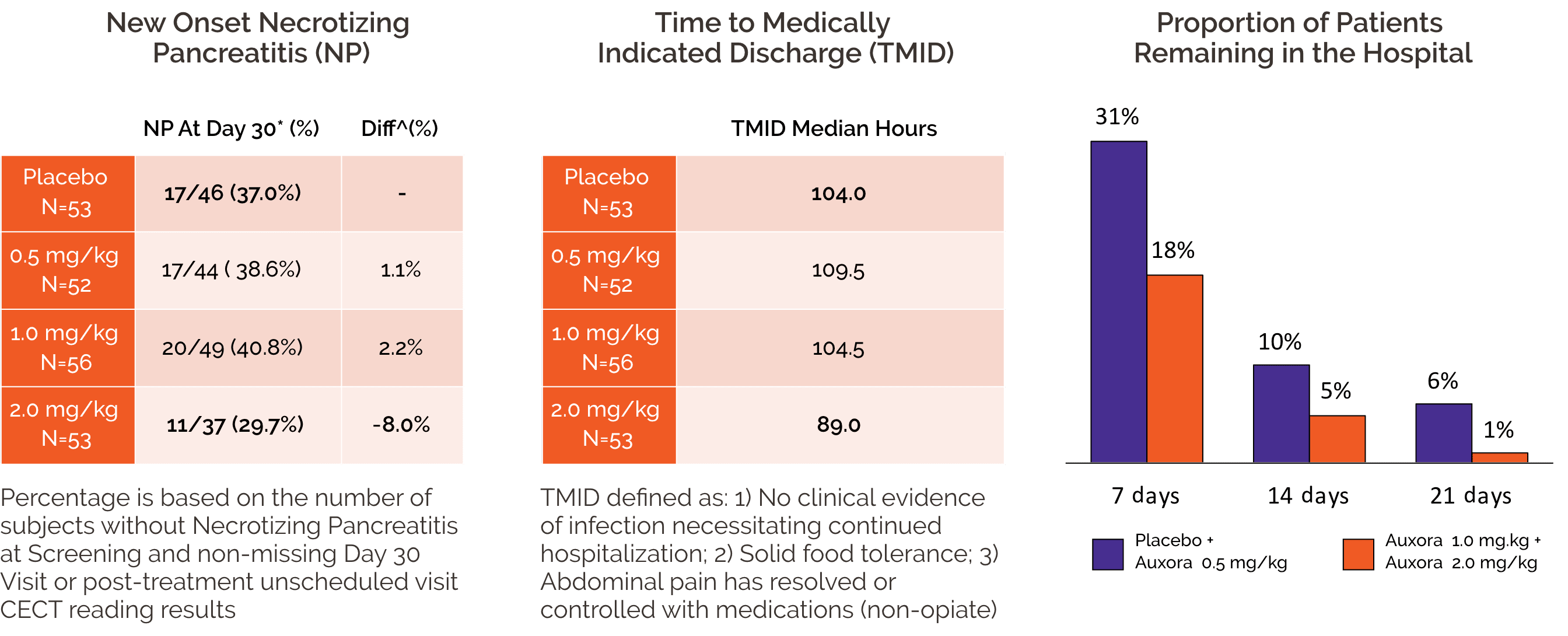
*If the Day 30 visit data was missing, the last available unscheduled post-treatment data was used for Day 30 analysis based on the LOCF method.
^Cochran-Mantel-Haenszel test stratified by CRF recorded gender (male or female) and the risk for HCT (higher or lower) based on CRF data.
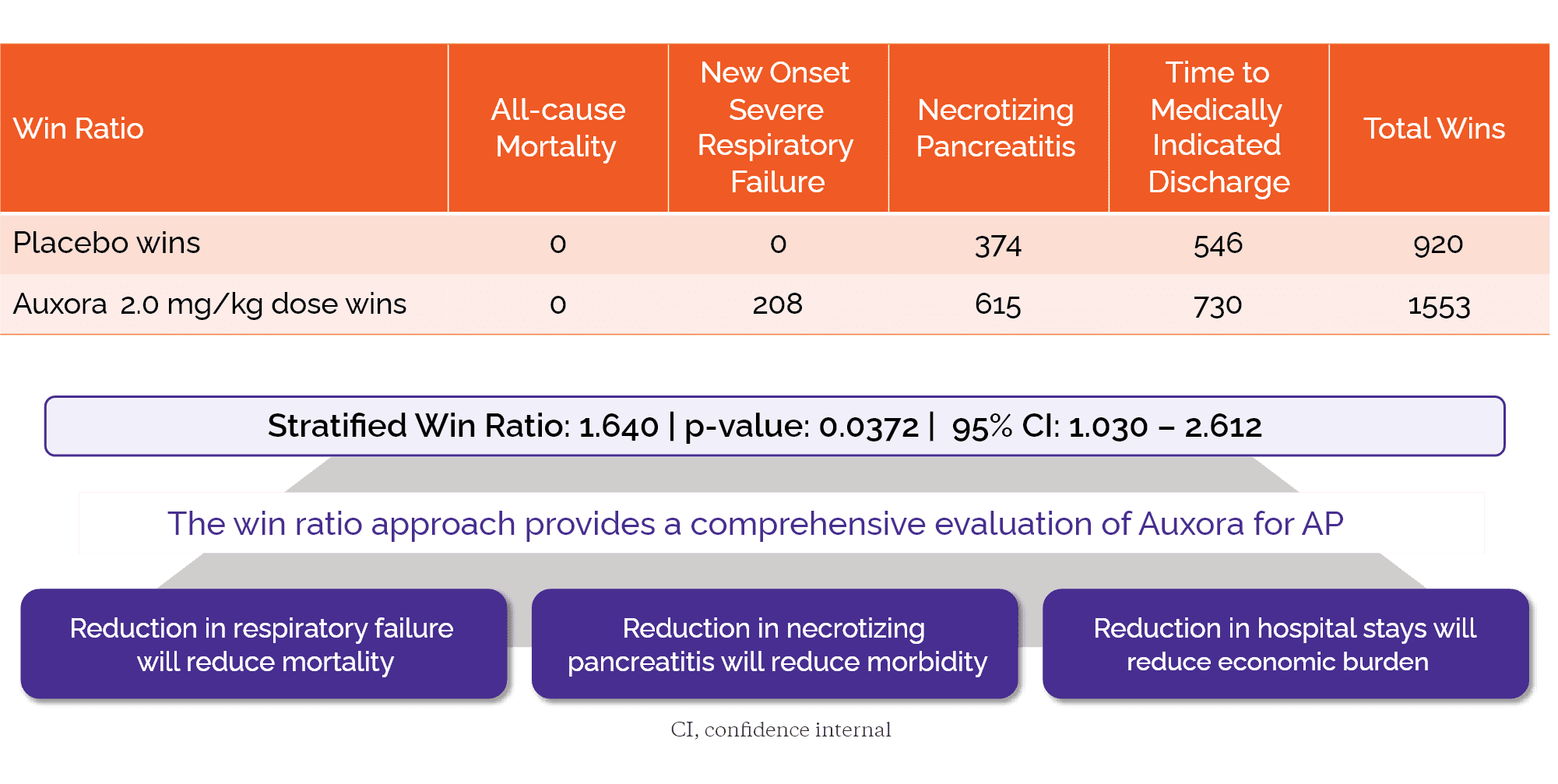
Integration of Key Endpoints into Win Ratio Demonstrates Potential Efficacy of Auxora High-Dose Compared to Placebo


Asparaginase-Induced Pancreatic Toxicity (AIPT)
Despite tremendous progress in treating acute lymphoblastic
leukemia (ALL) patients, significant toxicities from standard
drug therapies present the risk of serious on-going health
issues for some patients.
Current therapies result in long-term survival for over 90%
of pediatric ALL patients and one of the mainstays of therapy
in these patients is asparaginase, an enzyme that degrades
the amino acid asparagine, which is essential for the leukemic
cells to survive.
However, the administration of asparaginase triggers the
development of asparaginase-induced pancreatic toxicity (AIPT)
also known as asparaginase-associated pancreatitis (AAP)
in 7-10% of patients with ALL, with more than half of those
patients developing pancreatic necrosis or pseudocysts.
There are no approved therapeutics for AIPT/AAP.
pediatric patients treated for ALL per year in the U.S.
of AIPT patients develop pancreatic necrosis and/or pseudocysts
Current therapies for acute lymphoblastic leukemia (ALL) result in long-term survival for over 90% of pediatric ALL patients. One of the mainstays of therapy in these patients is asparaginase, an enzyme that degrades the amino acid asparagine, which is essential for the leukemic cells to survive.
However, the administration of asparaginase triggers the development of asparaginase-induced pancreatic toxicity (AIPT) also known as asparaginase-associated pancreatitis (AAP) in 7-10% of patients with ALL, with more than half of those patients developing pancreatic necrosis or pseudocysts.


Auxora™: Solving The Unmet
Need For Patients With Acute
Pancreatitis With SIRS and AIPT
Three to four Auxora™ infusions in the first 72-96 hours in our Phase 2a clinical trial of Auxora™ in 21 patients with acute pancreatitis: seven of 14 (50%) Auxora™ patients tolerated solid food after 72 hours, while only one of seven (14%) standard of care patients tolerated solid food. At the time of hospital discharge, 13 of 14 (93%) Auxora™ patients tolerated solid food compared to three of seven (43%) standard of care patients.
Auxora™ has the potential to:
• Enable earlier tolerance of solid food
• Allow for fewer days in hospital or ICU
• Reduce progression to organ failure
• Reduce progression to pancreatic necrosis


Three-four Auxora™ infusions in the first 72 hours in our Phase 2a clinical trial of Auxora™ in 21 patients with acute pancreatitis: seven of 14 (50%) Auxora™ patients tolerated solid food after 72 hours, while only one of seven (14%) standard of care patients tolerated solid food. At the time of hospital discharge, 13 of 14 (93%) Auxora™ patients tolerated solid food compared to three of seven (43%) standard of care patients.
Auxora™ has the potential to:
• Enable earlier tolerance of solid food
• Allow for fewer days in hospital or ICU
• Reduce progression to organ failure
• Reduce progression to pancreatic necrosis
Potential to Offer Significant Clinical Benefits to Children with AIPT
Auxora™ has the potential to rapidly resolve asparaginase-induced pancreatic toxicity (AIPT) in pediatric patients being treated for acute lymphoblastic leukemia (ALL), preventing development of further complications such as pancreatic necrosis and pseudocysts.
Our Pipeline
AIPT
CRSPA, an investigator led Phase 1/2 trial, is being conducted in children who develop AIPT, a toxicity of the chemotherapeutic asparaginase, in the course of their treatment for ALL. The first cohort of nine patients in this trial has been completed and, based on preliminary, unpublished data, all patients who received a full course of therapy had rapid resolution of their symptoms. We expect data from this trial to be published in 2023.
CRSPA Phase 1/2 Clinical Trial
Study Design
CRSPA Phase 1/2 clinical trial in children developing Asparaginase-Induced Pancreatic Toxicity (AIPT) resulting from treatment for Acute Lymphoblastic Leukemia (ALL)
Results
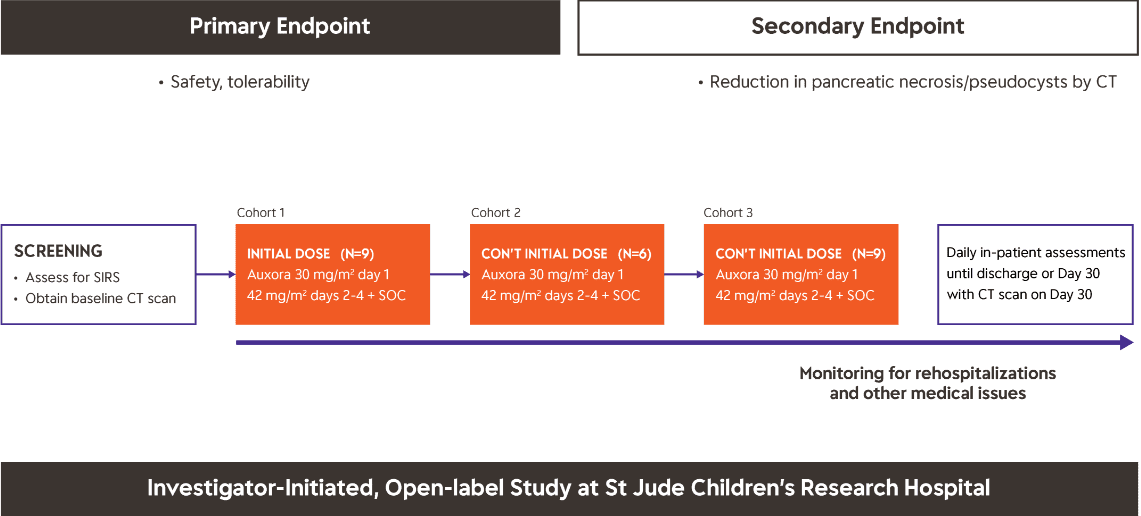
An investigator-sponsored Phase 1/2 clinical trial (CRSPA) at St. Jude Children’s Research Hospital (SJCRH) is investigating Auxora™ as a potential therapy in pediatric patients that develop AIPT due to the toxicity of the treatment for their underlying ALL.
This study is expected to provide valuable information on the use of Auxora™ in critically ill pediatric patients. Patients enrolled in this trial are treated with four daily doses of Auxora™ with the primary endpoints of safety, tolerability, and reduction in development of complications of AIPT, including pancreatic necrosis and pseudocysts.
For more details, please visit: Study of Auxora to Reduce the Severity of Pancreatitis Due to Asparaginase.
Information on our Expanded Access Policy can be obtained through the following link.
Potential to Offer Significant Clinical Benefits to Children with AIPT
Auxora™ has the potential to rapidly resolve asparaginase-induced pancreatic toxicity (AIPT) in pediatric patients being treated for acute lymphoblastic leukemia (ALL), preventing development of further complications such as pancreatic necrosis and pseudocysts.
Our Pipeline
AIPT
CRSPA, an investigator led Phase 1/2 trial, is being conducted in children who develop AIPT, a toxicity of the chemotherapeutic asparaginase, in the course of their treatment for ALL. The first cohort of nine patients in this trial has been completed and, based on preliminary, unpublished data, all patients who received a full course of therapy had rapid resolution of their symptoms. Results from this clinical trial are expected in the first half of 2024.
Chronic Pancreatitis is a progressive inflammatory disorder that leads to severe damage to the pancreas.
Chronic Pancreatitis
Chronic pancreatitis is a progressive inflammatory disorder that leads to severe damage to the pancreas, preventing the body from producing digestive enzymes. It also damages the insulin and other hormone-producing cells of the pancreas. The current standard of care for chronic pancreatitis, enzyme replacement therapy and diabetes medications, treats these symptoms but does not affect the underlying disease process.
There are no approved therapeutics for Chronic Pancreatitis.


Oral CRAC channel inhibitors.
Solving The Unmet Need For
Patients With Chronic
Inflammatory Disease, such as
Chronic Pancreatitis
Beyond Auxora, we are also developing CRAC channel inhibitors for use in chronic inflammatory indications such as chronic pancreatitis that would be administered as oral agents. We are currently conducting IND-enabling preclinical testing on several CRAC channel inhibitors for use in chronic inflammatory diseases.
Individuals in the U.S.
Increased risk of:
- Pancreatic cancer
- Diabetes
- Gallstones
- Kidney failure
- Malnutrition
- Breathing problems
Beyond Auxora, we are also developing CRAC channel inhibitors for use in chronic inflammatory indications such as chronic pancreatitis that would be administered as oral agents. We are currently conducting IND-enabling preclinical testing on several CRAC channel inhibitors for use in chronic inflammatory diseases.


Oral CRAC channel inhibitors.
Solving The Unmet Need For
Patients With Chronic
Inflammatory Disease, such as
Chronic Pancreatitis
Beyond Auxora, we are also developing CRAC channel inhibitors for use in chronic inflammatory indications such as chronic pancreatitis that would be administered as oral agents. We are currently conducting IND-enabling preclinical testing on several CRAC channel inhibitors for use in chronic inflammatory diseases.